Kidney transplantation (KT) is the outcome of great advancement in medical science.
Kidney transplantation is the treatment of choice for end-stage kidney disease (ESKD). Successful kidney transplantation may offer better quality of life and longer patient survival compared with dialysis. Life after successful kidney transplantation is almost normal.
Kidney transplantation is discussed in four parts:
- Pre-Transplant Information
- Transplant surgery
- Post Transplant care
- Deceased donor (Cadaveric) kidney transplant
1. Pre-Transplant Information
What is kidney transplantation?
Kidney transplantation is a surgical procedure in which a healthy kidney (from a living donor or deceased - cadaver donor) is placed into the body of a person suffering from end-stage kidney disease (recipient).
When is kidney transplant necessary?
Kidney transplantation is necessary for patients who are suffering from ESKD who are on dialysis (hemodialysis or peritoneal dialysis) or who are approaching ESKD but not yet on dialysis (pre-emptive KT).
When is kidney transplant not required in kidney failure?
A patient with acute kidney injury should not undergo KT. Kidney transplantation is also not done in cases where only one kidney fails and the other kidney is still functioning. Transplantation should only be done if the renal failure is irreversible.
Discovery of kidney transplantation has been a blessing for patients with chronic kidney failure.
Why is kidney transplant necessary in end-stage kidney disease?
Dialysis replaces some degree of the filtration of waste products of the kidneys. Other functions of the kidneys are not accomplished, some of which are better addressed by transplantation. Hence, kidney transplantation, when a suitable donor is available and when no contraindications are present, offers the best treatment option for complete rehabilitation of a patient with end-stage kidney failure. As kidney transplantation saves lives and enables one to enjoy almost normal life, it is referred to as the “Gift of Life”.
What are the advantages of kidney transplantation?
Major benefits of successful KT are:
- Better degree of replacement of renal function and better quality of life: The patient may achieve an almost normal and active lifestyle with more energy, stamina and productivity.
- Freedom from dialysis: Patients avoid the complications, cost, lost time and inconveniences of dialysis treatment.
- Longer life expectancy: Transplant patients have a longer life expectancy than risk-matched patients who remain on dialysis.
- Lesser dietary and fluid restrictions.
- Cost-effectiveness: Although the initial cost of a kidney transplant may be high, the expenses decrease by the second to third year post-transplant and by then, is usually less than that needed for maintenance dialysis treatment.
- There is a reported improvement in sexual life and a higher chance of fathering a child in males and becoming pregnant in females.
Successful kidney transplantation is the best treatment option for CKD-ESKD as it offers almost normal life.
What are the disadvantages of kidney transplantation?
Kidney transplantation offers many benefits but also has disadvantages. These are:
- Risk of major surgery. Kidney transplantation is a major surgical procedure under general anesthesia that has potential risks both during and after the surgery.
- Risk of rejection. There is no 100% guarantee that the body will accept the transplanted kidney. But with the availability of newer and better immunosuppressant drugs, rejections are less likely than they were in the past.
- Regular medication. Transplant patients will need to take immunosuppressive medicines regularly for as long as their donor kidneys are functioning. Discontinuation, missing or not taking the full dosage of immunosuppressant drugs, carries the risk of failure of transplanted kidney due to rejection.
- Risks related to immunosuppressive drugs: Drugs that suppress the immune response and rejection may lead to severe infections . Care to avoid infections and screening for development of some forms of cancer are part of post-transplant care. There are side effects for drugs like high blood pressure, high blood cholesterol and sugar levels.
- Stress. Waiting for a kidney donor before transplant, uncertainty of success of transplant (the transplanted kidney may fail) and fear of losing function of the newly transplanted kidney after transplant, is stressful.
- Initial high cost.
Kidney transplantation is not performed in CKD patients with AIDS, cancer and other serious diseases.
What are the contraindications for a kidney transplant?
Kidney transplantation is not recommended if the ESKD patient has:
- A serious active infection
- Active or untreated malignancy
- Severe psychological problems or mental retardation
- Unstable coronary artery disease
- Refractory congestive heart failure
- Severe peripheral vascular disease
- Antibodies against the donor kidney
- Other severe medical problems.
What is the age limit for a kidney transplant recipient?
Although there is no fixed criteria for the age of a kidney transplant recipient, it is usually recommended for persons from 5 to 65 years of age.
What are the likely sources of kidneys for transplantation?
There are three sources of kidneys for transplantation:
- Living related donors: blood relatives of the recipient up to the 4th degree of consanguinity.
- Living non-related donors: like friends, spouses or relatives.
- Deceased (cadaver) donors: from victims of brain death.
Who is the ideal kidney donor?
An identical twin is an ideal kidney donor with the best chances of survival after transplantation.
Kidney donated by family member donors results in most successful kidney transplantation.
84. Save Your Kidneys
Who can donate a kidney?
A healthy person with two kidneys can donate one kidney as long as the blood group, tissue type and tissue crossmatching are compatible with the receipient. Generally, donors should be between the ages of 18 and 65 years.
How does blood group determine the selection of a kidney donor?
Blood group compatibility is important in KT. The recipient and donor must have either the same blood group or compatible groups . Just like in blood transfusions, a donor with blood group O is considered a “universal” donor. (see table below)
| Recipient’s blood group |
Donor’s blood group |
| O |
O |
| A |
A or O |
| B |
B or O |
| AB |
AB,A, B or O |
Who cannot donate a kidney?
A living donor should be thoroughly evaluated medically and psychologically to ensure that it is safe for him or her to donate a kidney. A person cannot donate kidney if he or she has diabetes mellitus, cancer, HIV, kidney disease, high blood pressure or any major medical or psychiatric illness.
What are the potential risks to a living kidney donor?
A potential donor is evaluated thoroughly to ensure that it is safe for him or her to donate a kidney. With a single kidney, most donors live a normal healthy life. After kidney donation sexual life is not affected. A woman can have children and a male donor can father a child. Potential risks of kidney donation surgery are the same as those with any other major surgery. Risk of contracting kidney disease in kidney donors is not any higher just because they have only one kidney.
Kidney donation is safe and saves lives of CKD patients.
85. CHP. 14. Kidney Transplantation
What is paired kidney donation?
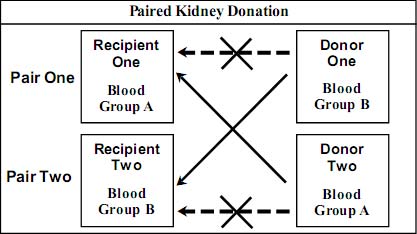 Living donor kidney transplantation has several advantages over deceased donor kidney transplantation or dialysis. Many patients with end-stage kidney disease have healthy and willing potential kidney donors but the hurdle is blood group or cross match incompatibility.
Living donor kidney transplantation has several advantages over deceased donor kidney transplantation or dialysis. Many patients with end-stage kidney disease have healthy and willing potential kidney donors but the hurdle is blood group or cross match incompatibility.
Paired kidney donation (also known as “live donor kidney exchange”, “living donor swap” or “kidney swap”) is the strategy which allows the exchange of living donor kidneys between two incompatible donor/ recipient pairs to create two compatible pairs.
This can be done if the second donor is suitable for the first recipient, and the first donor is suitable for the second recipient (as shown above). By exchanging the donated kidneys between the two incompatible pairs, two compatible transplants can be performed.
What is pre-emptive kidney transplant?
Kidney transplantation usually takes place after a variable period of dialysis therapy. Kidney transplantation may be done before the initiation of maintenance dialysis when the renal function is less than 20 ml/min. This is called a pre-emptive KT.
Pre-emptive KT is considered the best option for kidney replacement therapy in medically suitable patients with end stage kidney disease (ESKD) because it not only avoids the risks, cost, and inconvenience of dialysis, but also is associated with better graft survival than transplantation performed after initiating dialysis. Because of its benefits, one is strongly advised to consider a pre-emptive transplantation in ESKD, if a suitable donor is available.
86. Save Your Kidneys
2. Transplant Surgery
How is a kidney transplanted?
Before surgery, medical, psychological and social evaluation is done to ensure fitness and safety of both the recipient and the donor (in living-kidney donor transplant). Testing also ensures proper blood group and HLA matching and tissue crossmatching.
 Kidney transplantation is a teamwork of the nephrologists, transplant surgeon, pathologist, anesthesiologist and supporting medical (cardiologist, endocrinologist, etc) and nursing staff as well as transplant coordinators.
Kidney transplantation is a teamwork of the nephrologists, transplant surgeon, pathologist, anesthesiologist and supporting medical (cardiologist, endocrinologist, etc) and nursing staff as well as transplant coordinators.
After a thorough explanation of the procedure a careful reading of the consent form, consent of both the recipient and the donor (in living kidney donation) is obtained.
In living-kidney donor transplant surgery, both the recipient and the donor are operated on simultaneously.
This major surgery lasts from three to five hours and is performed under general anesthesia.
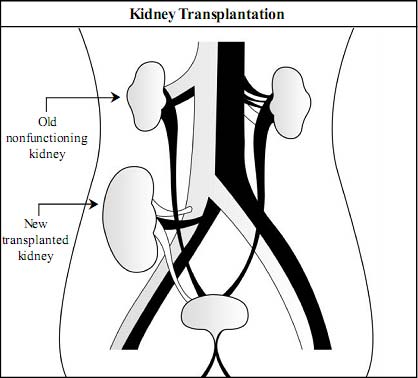
In living-kidney donor transplant surgery, usually the left kidney is removed from the donor either by open surgery or by laparoscopy. After removal, the kidney is washed with a special cold solution and subsequently placed into the right lower (pelvic) part of the abdomen of the recipient.
In most cases, the old diseased kidneys of the recipient are not removed.
When the source of kidney is a living donor, the transplanted kidney usually begins functioning immediately. However, when the source of the kidney is a deceased (cadaver) kidney donor, the transplanted kidney may take a few days or weeks to begin functioning. The recipient with delayed functioning transplanted kidney needs dialysis until kidney function becomes adequate.
After the transplant, the nephrologist supervises the monitoring and medications of the recipient. Living donors should also be screened and monitored regularly for any health issues that may develop.
In kidney transplantation, kidney is transplanted in lower abdomen of the recipient without disturbing old kidneys.
88. Save Your Kidneys
3. Post-Transplant Care
What are the likely post-transplant complications?
The common possible complications after transplantation include rejection, infection, medication side effects and post-operative complications. Major considerations in post-transplant care are:
- Post-transplant medications and kidney rejection.
- Precautions to keep the transplanted kidney healthy and to prevent infections.
Post-transplant Medications and Kidney Rejection
How does post-surgical management of kidney transplantation differ from other routine surgery?
In most cases of routine surgery, post-surgical medications and care are needed for about 7-10 days. However, after kidney transplantation, lifelong regular medications and meticulous care are mandatory.
What is kidney rejection?
The immune system of the body is designed to recognize and destroy foreign proteins and antigens like harmful bacteria and viruses. When the recipient’s immune system recognizes that the transplanted kidney is not ‘its own,’ it attacks the transplanted kidney and tries to destroy it.
89. CHP. 14. Kidney Transplantation
This attack by the body’s natural defense on a transplanted kidney is known as rejection. Rejection occurs when the transplanted kidney is not accepted by the body of the transplant recipient.
Major post-transplant complications are kidney rejection, infection and side effects of drugs.
When does kidney rejection occur and what is its effect?
Rejection of the kidney can occur at any time after the transplant, most commonly in the first six months. The severity of rejection varies from patient to patient. Most rejections are mild and easily treated by proper immunosuppressant therapy. In a few patients however, rejection may be severe not responding to therapy and eventually destroying the kidney.
What medications should a patient take after transplant to prevent rejection?
- Because of the immune system of the body, there is always a risk of rejection of the transplanted kidney.
- If the immune system of the body is suppressed the risk of rejection is decreased. However, the patient becomes prone to life-threatening infections.
- Special drugs are given to patients after kidney transplantation to selectively alter the immune system and prevent rejection, but minimally impair the ability of the patient to fight infections.
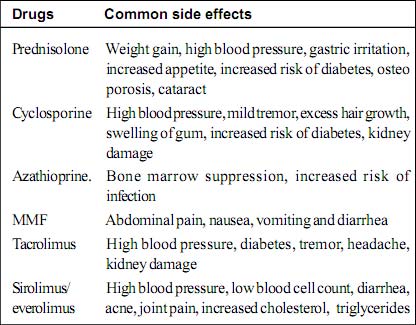
Such special drugs are known as immunosuppressant drugs. At present, the most widely used immunosuppressant drugs are tacrolimus/cyclosporine, mycophenolate mofetil (MMF), sirolimus/ everolimus and prednisolone.
How long does the patient need to continue immunosuppressant drugs after kidney transplant?
Immunosuppressant medications have to be given throughout life, for as long as the kidney graft is functioning. In the immediate post transplant period, several drugs are given but their numbers and dosages are gradually reduced over time.
After kidney transplantation lifelong drug therapy is mandatory to prevent kidney rejection.
 Does the patient need any other medication after kidney transplant?
Does the patient need any other medication after kidney transplant?
Yes. After kidney transplant, in addition to immunosuppressant drugs, antihypertensive drugs, calcium, and medications to treat or prevent infection and anti-peptic ulcer medications may be prescribed.
What are the common side effects of immunosuppressant drugs?
Common side effects of immunosuppressant drugs are summarized in the following table.
What happens if transplanted kidney fails?
When a transplanted kidney fails, the patient may either undergo a second transplant or undergo dialysis.
If a transplanted kidney fails, initiation of dialysis and a second transplant are two treatment options.
Precautions after kidney transplant
Successful kidney transplant provides a new, normal, healthy and independent life. However, the recipient must live a disciplined lifestyle and follow precautions to protect the transplanted kidney and prevent infections. The patient has to be compliant and take prescribed medications regularly and without fail.
General guidelines to keep transplanted kidney healthy
- Never stop taking medication or modify its dosage. Remember that irregularity, modification or discontinuation of medications are some of the most common reasons for transplant failure.
- Always keep a list of medications and maintain adequate stock. Do not take any over-the-counter drugs or herbal therapies.
- Blood pressure, volume of urine, weight and blood sugar (if advised by the doctor) every day.
- Regular follow up with a doctor and laboratory tests as advised, is mandatory.
- Get blood tested in reputed laboratories only. If laboratory reports are not satisfactory, rather than changing the laboratory, it is advisable to consult your doctor at the earliest.
- In an emergency, if you need to consult a doctor who is unaware about your disease, do not fail to inform him that you are a transplant recipient and brief him about the medications.
- There are less dietary restrictions after transplantation. Meals should be taken regularly. One should eat a well-balanced diet with adequate calories and proteins as prescribed. Eat foods low in salt, sugar, and fat and high in fiber to avoid weight gain.
Keys for success in post-transplant period are regularity, precautions and watchfulness.
- Water intake should be adequate to avoid dehydration. Patients may require up to more than three liters of water a day.
- Exercise regularly and keep weight under control. Avoid heavy physical activity and contact sports e.g. boxing, football.
- Safe sexual activities can be resumed after about two months, after consulting the doctor.
- Avoid smoking and alcohol intake.
- Stay away from crowded places such as cinemas, shopping malls, public transportation and people who have infections.
- Always wear a face mask in public places and high-risk areas such as construction sites dust-laden environments, excavation sites, caves, animal care settings, farms, gardens, etc.
- Always wash your hands with soap and water before you eat, before preparing or taking medications and after using the bathroom.
- Drink filtered boiled water.
- Eat fresh home-cooked cooked food in clean utensils. Avoid eating meals cooked outside the home and raw, uncooked foods. Avoid raw fruits and vegetables for the first 3 months after transplant.
- Maintain proper cleanliness at home.
- Take good care of teeth by brushing twice a day.
- Do not neglect any cuts, abrasions or scrapes. Promptly clean them with soap and water cover them with clean dressing.
Immediately consulting a doctor and promptly treating any new or unusual problem are mandatory to protect the kidney.
Consult or call the doctor or transplant clinic in case of:
- Fever over 100 F or 37.8 C and flu-like symptoms such as chills, body aches or persistent headache.
- Pain or redness over or around the transplanted kidney.
- Significant decrease in urine output, fluid retention (swelling) or rapid weight gain (more than 1 kg in a day).
- Blood in the urine or burning sensation during urination.
- Cough, breathlessness, vomiting or diarrhea.
- Development of any new or unusual symptoms.
- Immediately contacting the doctor and promptly treating any new or unusual problem are mandatory to protect the kidney.
Why are only a few patients with kidney failure able to get kidney transplants?
A kidney transplant is the most effective and best treatment option for patients with chronic kidney disease - end stage kidney failure. There is a large number of patients who need or wish to obtain a kidney transplant. There are three important reasons for the limited feasibility of the procedure.
- Unavailability of kidney:Only a few patients are luckyto obtain either living (related or non-related) or deceased (cadaveric) kidney donors. Major problems are the limited availability of living donors and the long waiting list for deceased donors.
- Cost:The cost of transplant surgery and the post-transplant lifelong medications is very high. This is a major hurdle for a large number of patients in developing countries.
- Lack of facilities: In many developing countries, facilities for kidney transplantation are not readily or easily available.
The scarcity of kidney donors is a major hurdle which deprives patients from the benefits of a transplant.
4. Deceased (Cadaveric) Kidney Transplantation
What is deceased kidney transplantation?
Deceased (cadaver) transplantation involves transplanting a healthy kidney from a patient who is “brain dead” into a patient with CKD. The deceased kidney comes from a person who has been declared “brain dead” with the desire to donate organs having been expressed either by the family or by the patient previously, at the event of his/her death.
Why are deceased kidney transplants necessary?
Due to the shortage of living donors, many CKD patients, though keen to have a transplant, have to remain on maintenance dialysis. The only hope for such patients is a kidney from deceased or cadaver donors. The most noble human service is being able to save the lives of others after death by donating organs. A deceased kidney transplant also helps eliminate illegal organ trade and is the most ethical form of kidney donation.
What is “Brain Death”?
“Brain death” is the complete and irreversible cessation (stopping) of all brain functions that leads to death. The diagnosis of “brain death” is made by doctors in hospitalized unconscious patients on ventilator support.
In “Brain Death” damage is irreversible with no chances of improvement by any medical or surgical treatment.
Criteria for diagnosis of brain death are:
- The patient must be in a state of coma and the cause of the coma (e.g. head trauma, brain hemorrhage etc) is firmly established by history, clinical examination, laboratory testing, and neuroimaging. Certain medications (e.g. sedatives, anticonvulsants, muscle relaxants, anti-depressants, hypnotics and narcotics), metabolic and endocrine causes can lead to an unconscious state that can mimic brain death. Such causes have to be excluded before confirming the diagnosis of brain death. The doctor should correct low blood pressure, low body temperature and low body oxygen before considering brain death.
- Persistent deep coma in spite of proper treatment under care of experts for an adequate period to “exclude the possibility of recovery”.
- No spontaneous breathing, patient is on ventilator support.
- Respiration, blood pressure and blood circulation is maintained with ventilator and other life support devices.
What is the difference between brain death and unconsciousness?
An unconscious patient may or may not need the support of a ventilator and is likely to recover after proper treatment. In a patient with “Brain Death,” the brain damage is severe and irreversible and is not expected to recover despite any medical or surgical treatment. In a patient with “Brain Death”, as soon as the ventilator is switched off, respiration stops and the heart stops beating. It is important to remember that the patient is already legally dead and removing the ventilator is not the cause of death. Patients with “Brain Death” cannot remain on ventilator support indefinitely, as their heart will stop relatively soon.
Is it possible to donate a kidney after dying?
No. Death occurs after the heart and respiration stop irreversibly and permanently. Like corneal donation, after death, kidney donation is not possible. When the heart stops, the blood supply to the kidney also stops, leading to severe and irreversible damage to the kidney, preventing its use for kidney transplantation.
In “Brain Death” the body’s respiration and blood circulation are artificially maintained after death.
What are the common causes for “Brain Death?”
Common causes of brain death are head injuries (i.e. falls or vehicular accidents), intracranial brain hemorrhage, brain infarct and brain tumor.
When and how is “Brain Death” diagnosed? Who diagnoses “Brain Death?”
When a deeply comatose patient kept on ventilator and other life supporting devices for an adequate period does not show any improvement on clinical and neurological examination, the possibility of “Brain Death” is considered. Diagnosis of brain death is made by a team of doctors who are not involved in kidney transplantation This team includes the attending physician, neurologist or neurosurgeon, who, after independent examinations of the patient, declare “brain death.” By detailed clinical examination, various laboratory tests, special EEG test for brain and other investigations, all possibilities of recovery from brain damage are explored. When no chance of any recovery is confirmed, “brain death” is declared.
What are the contraindications for kidney donation from a patient with “Brain Death?”
Under the following conditions a kidney cannot be accepted from a donor with brain death:
- A patient with active infections.
- A patient suffering from HIV or hepatitis B or C.
- A patient with long standing hypertension, diabetes mellitus, kidney disease or presence of kidney failure.
- Cancer patient (except brain tumor).
One deceased donor can save the lives of two CKD patients as he donates both his kidneys.
Which other organs can be donated by cadaver donors?
Cadaver donors can donate both kidneys and save lives of two patients. Besides kidney, other organs which can be donated are eye, heart, liver, skin, pancreas etc.
Who comprise the team for deceased kidney transplantation?
For deceased (cadaveric) kidney transplantation proper team work is necessary. The team includes:
- Relatives of the deceased kidney donor for legal consent.
- Attending physician of the donor.
- Cadaver transplant coordinator, who explains and helps the relatives of the patient for kidney donation.
- Neurologist who diagnoses the brain death.
- Nephrologist, urologist, transplant surgeon and team.
How is deceased kidney transplantation performed?
These are essential aspects of deceased kidney transplantation.
- A proper diagnosis of brain death is mandatory.
- The donor kidneys should be confirmed to be reasonably healthy and the donor should have no systemic disease that would contraindicate donation.
- Consent to donation should be given by a relative or person who is legally allowed to do so.
- Donor is kept on ventilator and other life-supporting devices to maintain respiration, heart beat and blood pressure until both kidneys are removed from the body.
After kidney transplantation the patient can enjoy a normal and active lifestyle.
98. Save Your Kidneys
- After removal, the kidney is processed properly with a special cold fluid and is preserved in ice. One deceased donor can donate both kidneys, so two recipients can be given the gift of life.
- Appropriate recipients are selected from a waiting list of patients following a protocol based on blood group, HLA matching and tissue cross matching compatibility.
- Better outcomes are expected the earlier the harvested kidneys are transplanted. They should ideally be transplanted within 24 hours of harvest. Beyond a certain length of time, they may not be viable for transplantation anymore.
- The surgical procedure on the recipient is the same for both living or deceased kidney donation.
- During the period of time between harvest and transplantation, the donor kidney sustains some damage due to lack of oxygen, lack of blood supply and cold exposure from storage in ice. Because of such injury, the kidney may not function immediately after transplantation and on occasion, short term dialysis support may be necessary while waiting for the donor kidney to recover and regain function.
Is there any payment made given to the donor’s family?
None. Giving another person a new lease on life is an invaluable gift. Being a donation, the donor or the donor’s family should not expect to receive any payment in exchange for the donated kidney, neither does the recipient need to pay anyone. The joy and satisfaction for this humanitarian gesture should be enough compensation for the donor or the family
Organ donation is a spiritual act. What can be more sacred than saving a life?