Urinary tract infection (UTI) is a common problem in children with short term and long term health problems.
Why do urinary tract infections require urgent attention and immediate treatment in children compared to adults?
Children with urinary tract infection need immediate attention because:
- UTI is a common cause of fever in children and ranks third among the most common infections in children after respiratory tract infection and diarrhea.
- Inadequate and delayed treatment may cause permanent kidney damage. Recurrent UTI causes kidney scars that in the long term can lead to high blood pressure, poor kidney growth and even chronic kidney disease.
- Because of its variable presentation, diagnosis of UTI is often missed. A high index of vigilance and suspicion are necessary for its diagnosis.
- There is a high risk of recurrence.
What are the predisposing factors for urinary tract infections in children?
The following are common risk factors for UTI in children:
- Having a shorter urethra makes UTI more common in girls.
- Wiping from back to front (instead of front to back) after coming from the toilet.
- Structural abnormality of the urinary tract (e.g. posterior urethral valve).
- The presence of congenital urinary tract anomalies such as vesicoureteral reflux (condition with an abnormal backward flow of urine from the bladder up the ureters and toward the kidneys) and posterior urethral valve.
- Uncircumcised boys are more likely to develop UTI than circumcised boys.
- Stone in the urinary tract.
- Other causes: constipation, poor perineal hygiene, prolonged catheterization or family history of UTI.
Symptoms of Urinary Tract Infection
Older children can complain if they have problems with urination. Common symptoms of urinary tract infections are the same in older children as those in adults and are discussed in Chapter 18.
Younger children are unable to complain. Crying while voiding, difficulty or pain when voiding, foul smelling urine and frequent unexplained fever are common complaints of children with UTI. Young children with UTI may also have poor appetite, vomiting or diarrhea, poor weight gain or weight loss, irritability or no symptoms at all.
Urinary tract infection is a common cause of fever in children.
178. Save Your Kidneys
Diagnosis of Urinary Tract Infection
Investigations performed in children with urinary tract infections include:
1. Basic investigations in urinary tract infection
- Screening tests for UTI: Urine microscopy or dipstick tests. Further
details are discussed in Chapter 18.
- Definitive diagnostic test for UTI: Urine culture and sensitivity (Urine
CS) test for confirmation of diagnosis, identification of the specific bacteria causing infection and selection of the most appropriate
antibiotic for treatment.
- Blood tests: Hemoglobin, total and differential white cell count, blood
urea, serum creatinine, blood sugar and C reactive protein.
2. Investigations for diagnosis of risk factors of urinary tract
infection
- Radiological tests to detect underlying abnormalities: Ultrasound of
kidney and urinary bladder (KUB), X-rays of the abdomen, Voiding
Cystourethrogram (VCUG), CT scan or MRI of the abdomen and
Intravenous Urography (IVU).
- Tests to detect scarring of kidney: A dimercaptosuccinic acid
(DMSA) kidney scan is the best method for detecting kidney scarring.
DMSA scan should be done preferably 3 to 6 months after an
episode of UTI.
- Urodynamic studies to assess bladder function.
What is a voiding cystourethrogram? When and how is it
done?
- Voiding cystourethrogram or VCUG (previously known as
Micturating cystourethrogram or MCU) is a very important
diagnostic X-ray test for children with urinary tract infection and
vesicoureteral reflux (VUR). VCUG test is the gold standard for
the diagnosis of vesicoureteral reflux and its severity (grading), and
detection of abnormalities of the urinary bladder and urethra. It
should be done for every child below 2 years after the first episode
of UTI.
- VCUG should be done after treating UTI, usually after the first week
of diagnosis.
- In this test the urinary bladder is filled to its capacity with contrast
(radio opaque iodine containing dye fluid which can be seen on X-
ray films) through a catheter under strict aseptic precautions and
usually under antibiotic cover.
- A series of X-ray images are taken before and at timed intervals
during voiding. This test provides a comprehensive view of the
structure and the function of the bladder and urethra.
- VCUG can detect urine flow from the bladder backwards into the
ureters or kidneys, known as vesicoureteral reflux.
- VCUG is also used to detect the presence of a posterior urethral
valve in male infants.
Common symptoms of UTI in children are recurrent
fever, poor weight gain and urinary problems.
180. Save Your Kidneys
Prevention of Urinary Tract Infection
- Increasing fluid intake dilutes urine and helps in flushing out bacteria from the urinary bladder and urinary tract.
- Children should urinate every two to three hours. Holding urine in the bladder for a long period of time provides opportunity for bacteria to grow.
- Keep genital area of children clean. Wipe child from front to back (not back to front) after toilet. This habit prevents bacteria in the anal region from spreading to the urethra.
- Frequently change diapers to prevent prolonged contact of stool with the genital area.
- Children should be made to wear only cotton undergarments to allow air circulation. Avoid tight-fitting pants and nylon underwear.
- Avoid giving bubble baths.
- For the uncircumcised boy, the foreskin of his penis should be washed regularly.
- In children with VUR, recommend double or triple voiding (passing of urine) to prevent residual urine.
- A low dose daily antibiotic for long-term as a preventive (prophylactic) measure is recommended for some children who are prone to chronic UTI.
VCUG is the most reliable X-ray test used in children with UTI to detect vesicoureteral reflux and posterior urethral valve.
Treatment of Urinary Tract Infection
General measures
All preventive measures for urinary tract infection should be followed.
- A child with UTI should be advised to drink more water. Sick hospitalized children need intravenous fluid therapy.
- Appropriate medications should be given for fever.
- Urinalysis and urine culture and sensitivity should be done after completion of treatment to ensure that infection is controlled adequately. Regular follow up with urine tests is necessary for all children to confirm that there is no recurrence of infection.
- Ultrasound and other appropriate investigations should be done for all children with UTI.
Specific treatment
- In children, UTI should be treated with antibiotics without delay to protect the developing kidneys.
- Urine culture should be sent before initiating treatment to identify causative bacteria and properly select antibiotics.
- A child needs hospitalization and intravenous antibiotics if he/ she has high grade fever, vomiting, severe flank pain and is unable to take medicine by mouth.
- Oral antibiotics may be given to children more than 3 to 6 months of age who are able to take oral medications.
- It is important that children complete a full course of prescribed antibiotics, even if the child no longer has symptoms of UTI.
Recurrent urinary tract infection
Children with recurrent, symptomatic UTI need additional tests such as ultrasound, VCUG and at times DMSA scan to identify the underlying cause. Three important treatable problems for recurrent UTI are VUR, the posterior urethral valves and kidney stones. According to the underlying cause, specific medical treatment followed by preventive measures and long term preventive antibiotics therapy is planned. In some children surgical treatment is planned jointly by the nephrologist and urologist.
Inadequate and delayed treatment of UTI in children can cause irreversible kidney damage.
182. Save Your Kidneys
Posterior Urethral Valves
Posterior urethral valve (PUV) is a congenital abnormality of the urethra
which occurs in boys. It is the most common cause of obstruction of
the lower urinary tract in boys.
Basic problem and its importance: Folds of tissue within the urethra
lead to incomplete or intermittent blockage to the normal flow of urine
in PUV. A blockage to the urine flow through the urethra causes back
pressure on the urinary bladder. The size of the bladder increases
considerably and its muscle wall becomes very thick.
A very large urinary bladder with elevated bladder pressure leads to an increase in pressure which is felt by the ureters and kidney. This results
in dilatation (widening) of the ureters and the pelvocalyceal (drainage)
system of the kidneys. Such dilatation, if not diagnosed and treated
timely, can lead to chronic kidney disease (CKD) in the long term.
About 25% to 30% children born with PUV are likely to suffer from
end stage kidney disease (ESKD). PUV is therefore a significant cause
of morbidity and mortality in infants and children.
PUV causes obstruction of the lower urinary tract
in boys leading to CKD if not treated in time.
CHP. 23. Urinary Tract Infection in Children 183.
Symptoms:
Common symptoms of posterior urethral valves are weak
urine stream, dribbling of urine, difficulty or straining to when voiding ,
bedwetting, fullness of the lower part of the abdomen (supra pubic
region) due to a palpable urinary bladder and urinary tract infection.
Diagnosis: Ultrasound before birth (antenatal) or after birth in a male
child provides the first clue for the diagnosis of PUV. Confirmation of
the diagnosis of PUV requires the VCUG test that is carried out in the
immediate postnatal period.
Treatment:
Surgeons (urologists) and kidney specialists (nephrologists)
jointly treat PUV. The first treatment for immediate improvement is to
insert a tube into the urinary bladder (usually through the urethra and
occasionally directly through the abdominal wall - suprapubic catheter)
to drain urine continuously. Simultaneous supportive measures such as
treatment of infection, anemia and kidney failure; and correction of
malnutrition, fluid and electrolyte abnormalities help in the improvement
of the general condition.
Definitive treatment of PUV is surgical removal of the valve with the
use of an endoscope. All children need regular lifelong follow up with a
nephrologist subsequently because of the risk of UTI, problems of
growth, electrolyte abnormalities, anemia, high blood pressure and
chronic kidney disease.
Send urine for CS before initiating therapy to identify
causative bacteria & select appropriate antibiotics.
184. Save Your Kidneys
Vesicoureteral Reflux (VUR)
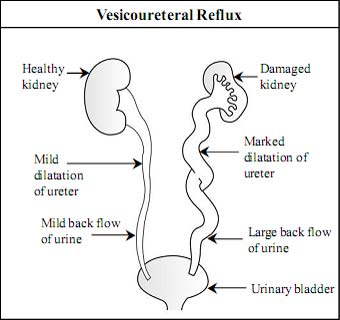
Vesicoureteral reflux (VUR) is “backward flow of urine from bladder into ureter”.
Why is it important to know about vesicoureteral reflux?
VUR is present in about 30 to 40 % of children with UTI associated with fever. In many children VUR may cause scarring and damage to the kidneys. Kidney scarring for a long period may cause high blood pressure, toxemia of pregnancy in young females, chronic kidney disease and, in a few patients, end stage kidney disease. VUR is more common in family members of a person with VUR and affects girls more frequently.
What is vesicoureteral reflux and why does it occur?
VUR is a condition with an abnormal backward flow (reflux) of urine from the bladder toward the ureters and possibly up to the kidneys. This can happen on either one or both sides.
Urine formed in kidneys flows down to the urinary bladder through the ureters. Urine normally flows in one direction, down the ureters and into the urinary bladder.
During urination and when the urinary bladder is filled with urine, a valve between the bladder and ureter is responsible for the prevention of back flow of urine into the ureters. VUR is caused by a defect in the mechanism of this valve.
VUR can be graded from mild to severe (Grade I to V) based on the severity of back flow of urine from the urinary bladder to the ureters and kidneys.
VUR is very common in children with UTI and carries the risk of hypertension and CKD.
CHP. 23. Urinary Tract Infection in Children 185.
 What causes vesicoureteral reflux?
What causes vesicoureteral reflux?
There are two types of VUR: primary VUR and secondary VUR. Primary VUR is the most common type of VUR and is present at birth. Secondary VUR can occur at any age. It commonly occurs due to obstruction or malfunction in the bladder or urethra with bladder infection.
What are the symptoms of vesicoureteral reflux?
There are no specific signs and symptoms of VUR. But frequent and recurrent urinary tract infection (UTI) is the most common presentation of VUR. In older children with untreated severe vesicoureteral reflux, signs and symptoms are apparent because of complications such as high blood pressure, protein in urine or kidney failure.
How is vesicoureteral reflux (VUR) diagnosed?
Investigations performed in children with suspected VUR are:
1. Basic diagnostic test for VUR
Voiding cystourethrogram
- VCUG is the gold standard for the diagnosis of vesicoureteral reflux and its severity (grading).
- Vesicoureteral reflux is graded according to the degree of reflux. The grade of VUR indicates how much urine is flowing backward into the ureters and kidneys. Grading is important in determining prognosis and most appropriate therapy for a given patient.
- In the mild form of VUR, urine refluxes only to the ureter (Grade I and II). In the most severe form of VUR there is massive reflux of urine, with marked tortuosity and dilatation of the ureter and severe kidney swelling (Grade V).
2. Additional investigations in VUR
- Urine test and urine culture: used to detect a urinary tract infection.
- Blood tests: basic tests usually performed are hemoglobin, white blood cells and serum creatinine. Serum creatinine can be used as a measure of kidney function.
- Kidney and bladder ultrasound: to find out the size and shape of the kidneys and to detect scars, kidney stones, obstruction or other abnormalities. It cannot detect reflux.
- DMSA kidney scan: this is the best method for detecting kidney scarring.
How is vesicoureteral reflux treated?
It is important to treat VUR to prevent possible infections and kidney damage. The management of vesicoureteral reflux depends on the grade of reflux, age of children and symptoms. There are three treatment options for VUR, : antibiotics, surgery and endoscopic treatment. The most common first-line treatment of VUR is the use of antibiotics to prevent UTI. Surgery and endoscopic treatment is reserved for severe VUR or in those cases where antibiotics have not been effective.
With regular antibiotics for a long term (years), low-grade reflux resolves without surgery.
CHP. 23. Urinary Tract Infection in Children 187.
Mild VUR: Mild VUR will resolve completely on its own by thetime a child is 5 to 6 years old. Children with mild VUR are less likely to need surgery. In such patients, a low dosage of antibiotics is given once or twice a day for a prolonged period of time to prevent UTI. This is called antibiotic prophylaxis. Antibiotic prophylaxis is usually given until the patient is 5 years of age. Remember that antibiotics per se do not correct VUR. Nitrofurantoin and cotrimoxazole are preferred drugs for antibiotic prophylaxis.
All children with VUR should follow general preventive measures for UTI (discussed above) and regular frequent and double voiding. Periodic urine tests are needed to detect UTI. VCUG and ultrasound are repeated yearly to determine if reflux has subsided.
Severe VUR: The severe form of VUR is less likely to resolve on its own. Children with the severe form of VUR require surgery or endoscopic treatment. Correction of reflux by open surgery (ureteral reimplantation or ureteroneocystostorny) prevents the backflow of urine. The main advantage of surgery is its high success rate (88-99%). Endoscopic treatment is a second effective treatment modality for the severe form of VUR. The benefits of endoscopic technique are that it can be performed in an outpatient setting, takes just 15 minutes, has fewer risks and does not require any incision. Endoscopic treatment is done under general anesthesia. In this method with the help of an endoscope (lighted tube) a special bulking material (e.g. Dextranomer/ hyaluronic acid copolymer - Deflux) is injected into the area where the ureter enters the urinary bladder. Injection of the bulking material increases the resistance at the entry of the ureter and prevents urine from flowing back into the ureter. The success rate for resolution of reflux with this method is about 85 to 90%. Endoscopic treatment is a convenient treatment option in the earlier stage of VUR as it avoids long term use of antibiotics and the stress of living with VUR for years. Follow-up:All children with VUR should be regularly monitored with measurement of height, weight, blood pressure, urine analysis and other tests as recommended by his/her doctor.
Surgery and endoscopic treatment are indicated in severe VUR or when antibiotics are not successful.
188. Save Your Kidneys
When should a patient with UTI consult a doctor?
For children with urinary tract infection the doctor should immediately be consulted in case of:
- Persistent fever, chills, pain or burning during urination, foul-smelling urine or blood in the urine.
- Nausea or vomiting which prevents intake of fluid and medication.
- Dehydration due to poor fluid intake or vomiting.
- Pain in the lower back or abdomen.
- Irritability, poor appetite, failure to thrive or child is unwell.
Regular follow up is advised in VUR to assess blood pressure, growth, recurrence of UTI and damage to the kidneys.